A collaborative effort among researchers from Germans Trias i Pujol Research Institute (IGTP), Institut d’Investigació Sanitària Pere Virgili (IISPV), Universitat Rovira i Virgili (URV), and the CIBER of Hepatic and Digestive Diseases (CIBEREHD) has shed new light on the potential of extracellular vesicles (EVs) as a therapeutic option for inflammatory bowel disease (IBD). Their findings, published in the journal Clinical and Translational Medicine, underscore the advantages of mesenchymal stem cell-derived EVs (MSC-EVs) in addressing the complexities of IBD.
IBD, including Crohn’s disease and ulcerative colitis, is defined by chronic inflammation of the gastrointestinal tract driven by immune dysregulation. Although current therapies have improved outcomes, about half of patients require surgery within a decade of diagnosis, highlighting the urgency for innovative solutions.
The research emphasizes the benefits of MSC-EVs compared to traditional cell-based therapies. “MSC-EVs represent a promising alternative with lower risks of immunogenicity and tumorigenicity. They are also easier to store and handle, which adds to their clinical appeal,” said Dr. Josep Manyé, researcher at IGTP and CIBEREHD.
The review delves into preclinical studies demonstrating MSC-EVs’ ability to modulate immune responses, promote tissue regeneration, and reduce inflammation. Leveraging advanced techniques such as transcriptomics, proteomics, and lipidomics, the team analyzed how these vesicles could restore intestinal balance. “We aimed to dissect their mechanisms of action to understand their role in chronic inflammation and tissue repair,” said Dr. Carolina Serena, principal investigator at IISPV.
The study also addresses the challenges of translating MSC-EV research into clinical practice, including the need for standardized characterization and isolation methods. “Our findings establish a robust platform for developing advanced therapies for IBD, offering safer and more effective options for patients,” noted Dr. Laura Clua-Ferré, first author and IGTP researcher.
While clinical trials investigating EVs for other conditions are underway, with around 20 in phase I or II, researchers stress the need to overcome regulatory and logistical hurdles before MSC-EV-based therapies can become a reality for IBD patients.
This work not only highlights the therapeutic promise of MSC-EVs but also reflects the dedication of the research community to advancing safer, more effective treatments for inflammatory bowel disease.
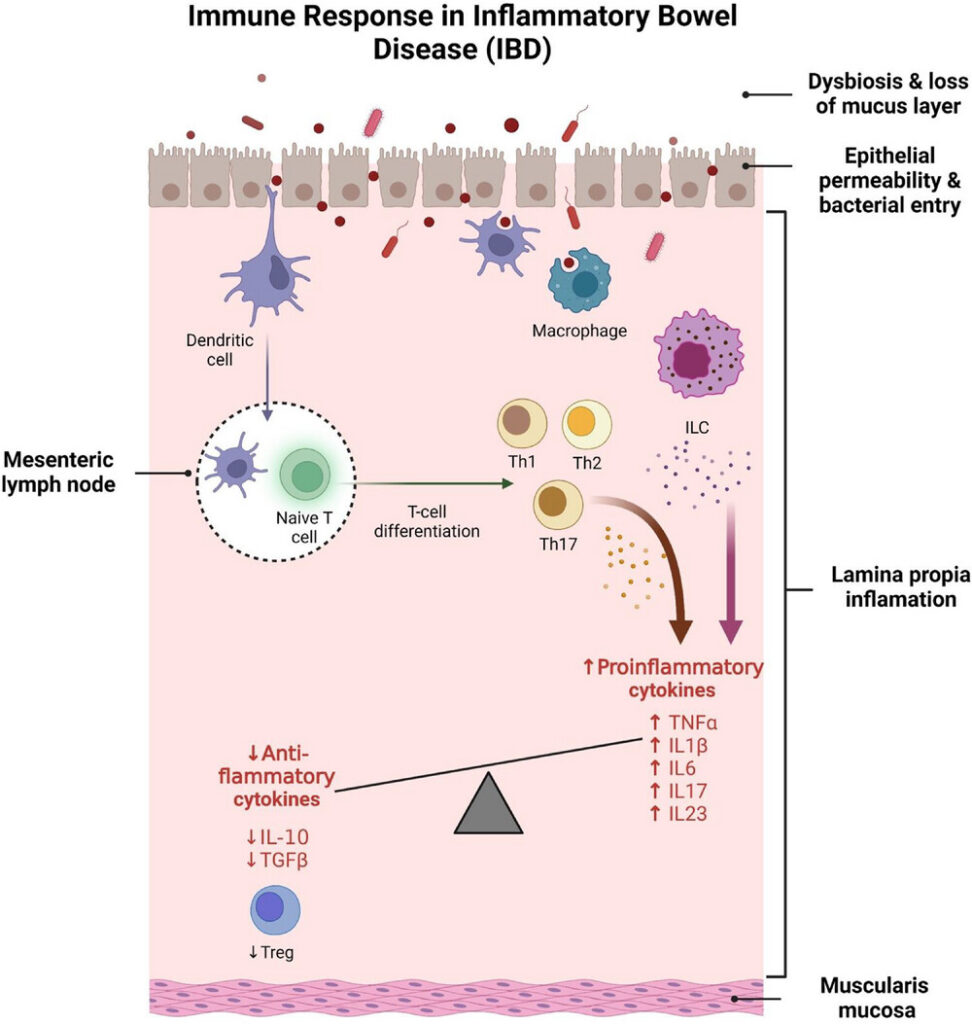
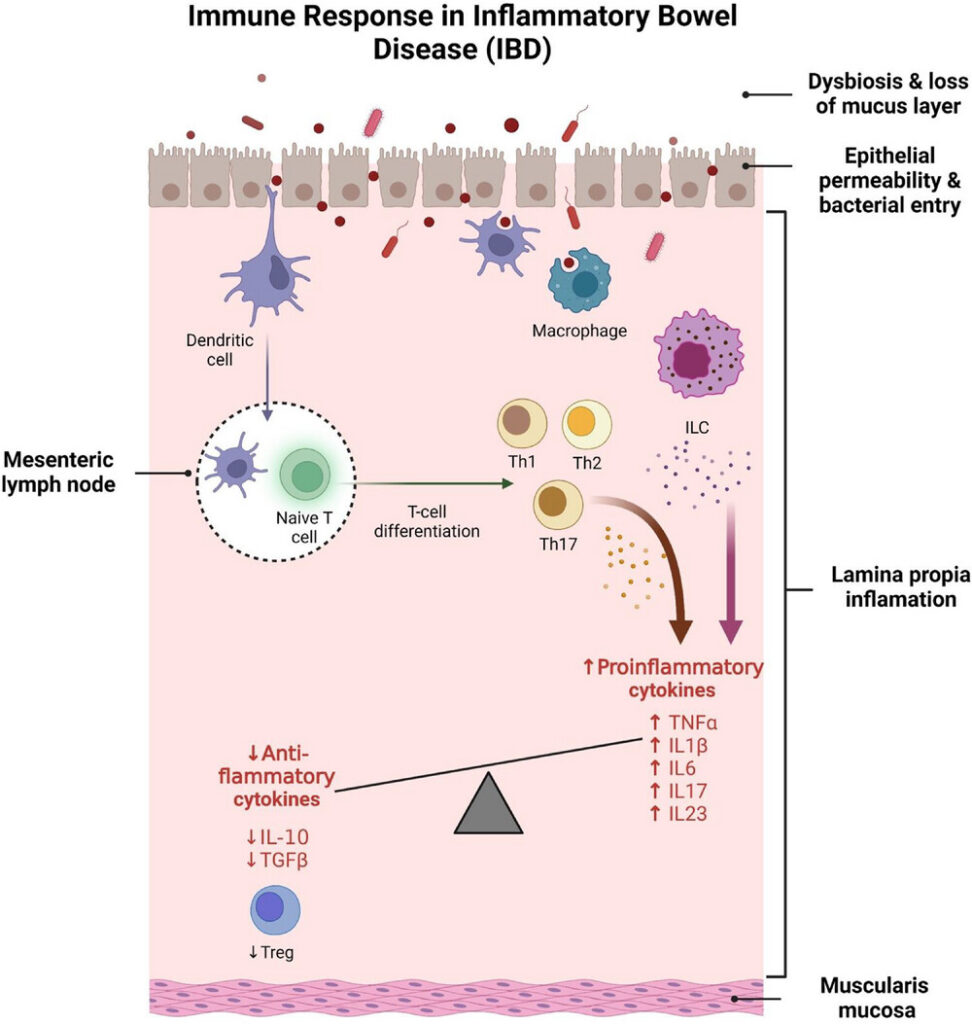
Figure Description:
Immune dysregulation and barrier dysfunction in the pathogenesis of inflammatory bowel disease (IBD). The disruption of intestinal homeostasis in IBD is driven by dysbiosis in the gut lumen, loss of the mucus layer, and increased epithelial permeability, allowing bacterial translocation into the lamina propria. Breaches in the epithelial barrier activate dendritic cells, which migrate to mesenteric lymph nodes and promote the differentiation of naïve T cells into pro-inflammatory T helper (Th) cell subsets. Under healthy conditions, regulatory T cells (Tregs) maintain immune homeostasis by secreting anti-inflammatory cytokines such as IL-10 and TGF-β. In IBD, this balance shifts toward pro-inflammatory Th cells, resulting in elevated levels of cytokines including TNF-α, IL-1β, IL-6, IL-17 and IL-23. Additionally, dysregulated innate lymphoid cells (ILCs) exacerbate IBD by producing IL-23, which stimulates IL-17 secretion, further driving inflammation.
Read the full paper.
Photo Credit: Clua-Ferré L, Suau R, Vañó-Segarra I, Ginés I, Serena C, Manyé J. Clin Transl Med. 2024